By Sharon Muza, BS, CD(DONA), BDT(DONA), LCCE, FACCE, CLE
A new research paper, Bearing witness: United States and Canadian maternity support workers’ observations of disrespectful care in childbirth, was recently published in the journal Birth. Written by Christine Morton, Ph.D., a medical sociologist and author and her colleagues, the study examines and compares the frequency with which birth doulas and labor and delivery nurses report witnessing disrespectful obstetrical care in the United States and Canada.
Introduction
Disrespectful care during labor and birth can have a lasting impact on the birthing person’s experience, long after the actual event has ended. One in four people giving birth in the U.S. today currently describes their birth as traumatic. Disrespectful care from health care providers during the experience can be a large contributor to the negative feelings that are experienced by people who have given birth.
Doulas and labor & delivery nurses are frequent witnesses to the behaviors and actions of the health care provider. This ongoing exposure to the disrespectful care shown to clients and patients can have a significant impact on the experience of the doulas and nurses, including moral distress, which may contribute to burnout, turnover, and poor quality of care.
The issue of disrespectful care in childbirth is receiving growing attention amongst consumers and professionals alike. There have been recent efforts to develop appropriate methods to document and quantify these behaviors. It has become apparent that racial and ethnic minorities are more likely to receive disrespectful treatment from their health care providers than their white counterparts. This group is already adversely impacted with higher rates of maternal and neonatal morbidity and mortality. When the scope and impact of the situation are appropriately understood, efforts can be implemented that focus on changing these behaviors.
The training (and responsibilities) of nurses and doulas are extremely different in scope. It is important to evaluate the experiences of observing disrespectful care in these two different groups. The specific role that each occupation fills may influence their observations of disrespectful care and the impact this disrespect has on them professionally and personally.
Here are the six types of disrespectful behaviors that the authors examined in this study: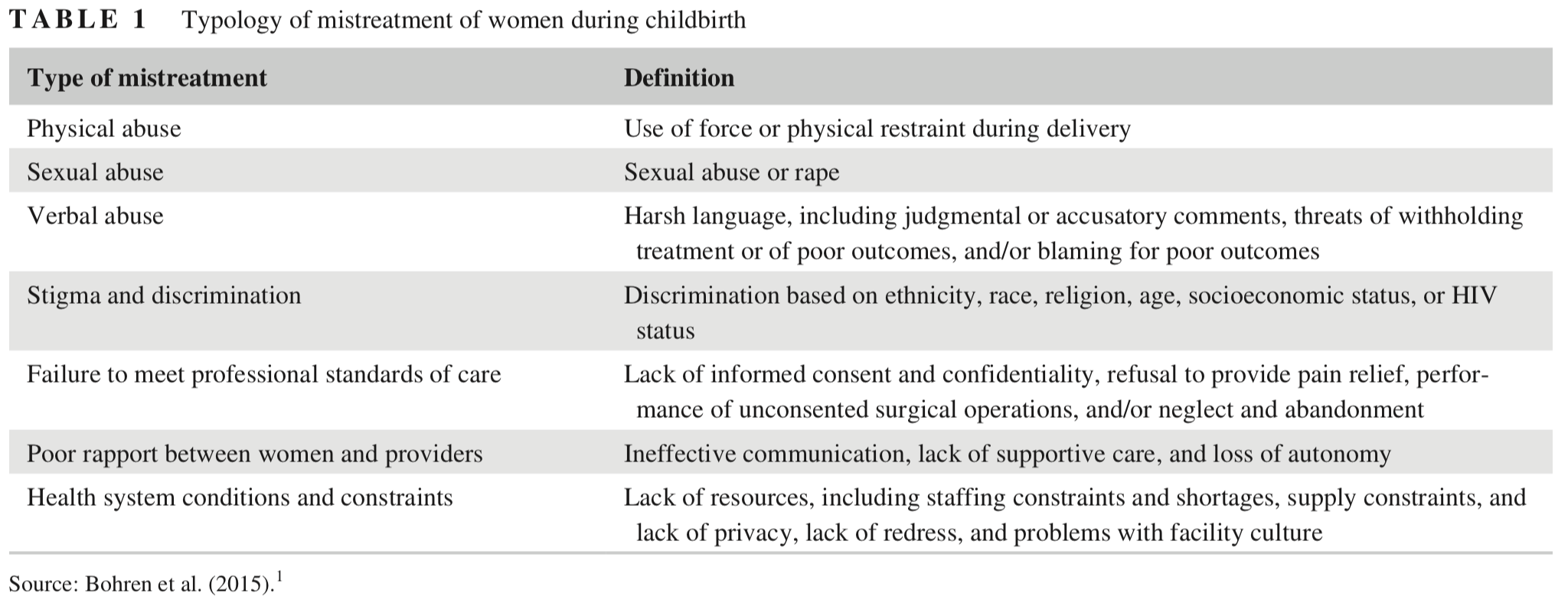 How the study was done
How the study was done
Data was obtained from the Maternity Support Survey, a 2012-2013 cross-sectional online survey of doulas and L&D nurses working in the United States and Canada. These two developed countries have been struggling with rising maternal mortality and recent reports of disrespectful care in childbirth. The survey asked how often respondents witnessed disrespectful care, including verbal abuse, discrimination, and violations of informed consent.
The researchers conducting this study examined the relationship between the doulas’ and L&D nurses’ demographic characteristics and the frequency with which they reported observing six types of disrespectful care. Survey participants were recruited through professional organizations, social media, and email. In addition to collecting demographic information, researchers also inquired about training, credentials, sources of knowledge about birth, financial rewards of and intention to leave maternity support work, childbirth and breastfeeding experiences, attitudes toward common labor practices, feelings of work-family conflict, work experiences including witnessing disrespectful care, work satisfaction and burnout, hospital characteristics, and understandings of informed consent and quality improvement initiatives. This paper documents how many doulas and L&D nurses witnessed healthcare providers demonstrating disrespectful behavior, how the rate differed based on profession, and what personal and experiential factors appear to influence that perception.
What were the results of the study?
A total of 1,435 doulas and 967 nurses were included in the study. Most doulas and nurses reported witnessing three of the six types of disrespectful care rarely or never but almost two-thirds (65.4%) reported witnessing a failure to provide informed consent as an occasional or frequent occurrence. One-third of all the respondents reported occasionally or often witnessing a care provider threatening a laboring person that their baby might die if they did not agree to a proposed procedure. Doulas reported seeing this more often than nurses. Approximately 10% of the respondents state that they witnessed racially or sexually demeaning language either occasionally or often. Doulas were 3.4% less likely to report witnessing racially demeaning language than nurses but were 4.7% more likely to say that they witnessed sexually degrading language. Almost 22% of respondents shared that they witnessed birthing people receiving more procedures because of their race/ethnicity, with 13.3% more doulas than nurses saying that this occurred occasionally or often.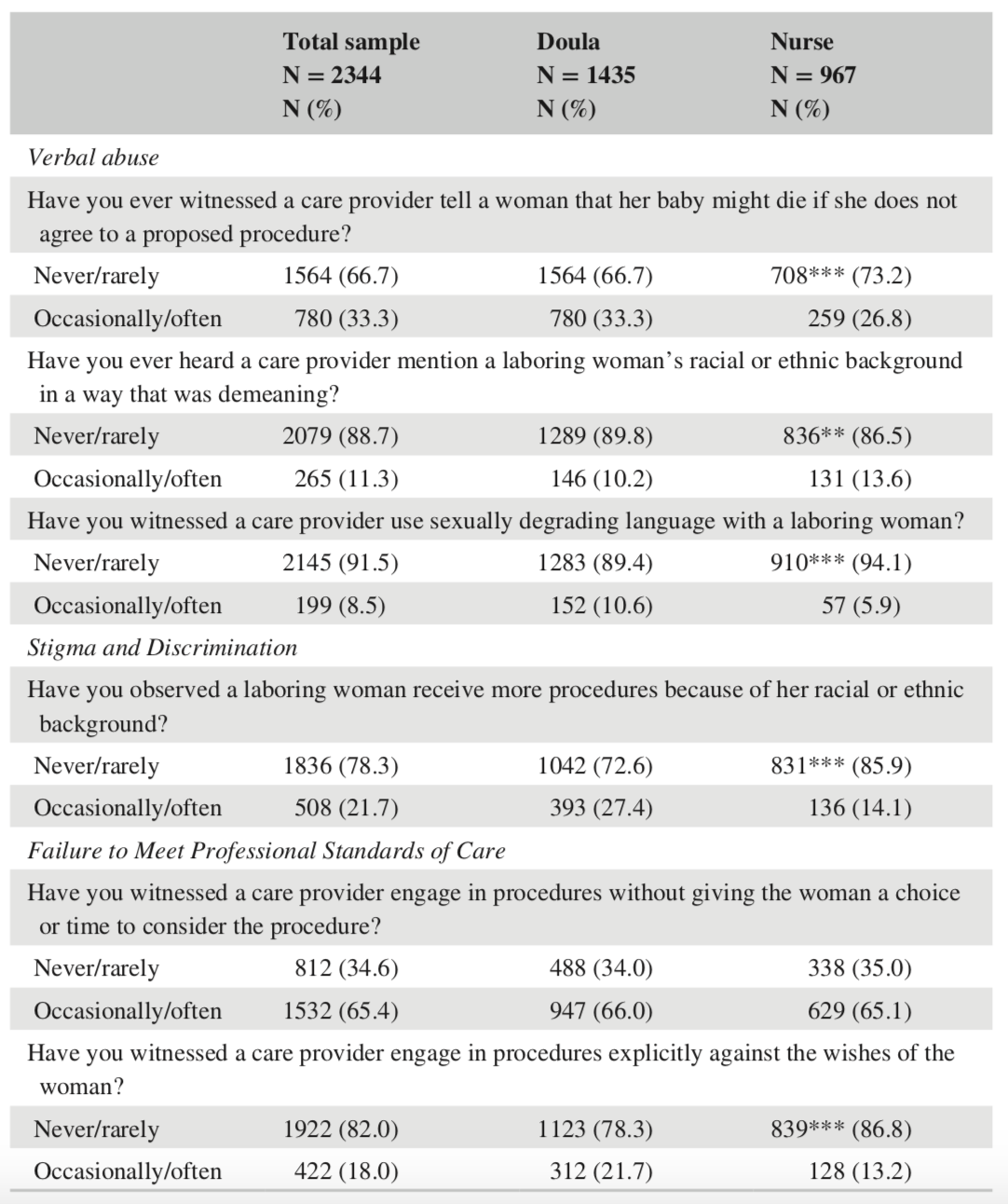
A failure to meet professional standards of care was the most common type of disrespectful care observed when evaluating study results. Overall, 65.4% of the doulas and nurses said that they had witnessed providers occasionally or often engaging in procedures without giving the laboring person sufficient time, or any time at all, to make a decision about whether they wanted to have the procedure. Eighteen percent of all respondents reported witnessing providers occasionally or often engaging in procedures explicitly against the patient’s wishes, and doulas were more likely to report witnessing this than nurses.
Other interesting results were that doulas and L&D nurses who had given birth were more likely to report witnessing threats that the baby might die, lack of informed consent, and care providers acting explicitly against a person’s wishes than those who had not given birth.
Doulas and nurses who planned to stop working in that role within three years were significantly more likely to report that they witnessed most types of disrespectful care either occasionally or often. Nurses and doulas who struggled with work-family conflict also had higher odds of reporting that providers occasionally or often threatened that a baby would die if a pregnant person refused a procedure, used extra procedures on some people based on their race/ethnicity, and failed to offer fully informed consent. Interestingly, there were some regional observations. Nurses and doulas in the Southern United States reported some types of disrespectful care (threats that the baby would die, lack of informed consent, and violations of informed consent) more often than those in the West.
Compared with doulas, nurses were less likely to report that providers threatened that a baby would die, used sexually degrading language, engaged in extra procedures based on race/ethnicity, and engaged in procedures explicitly against a person’s wishes.
What does this all mean?
This study provides new insights into doulas and nurses; observations of different categories of disrespectful care by health care providers. There were observable differences between the observations of the nurses and doulas. Approximately two-thirds of nurses and doulas reported occasionally or often witnessing providers fail to meet professional standards of care by engaging in procedures without obtaining informed consent or, less often, acting despite a pregnant person’s explicit refusal. This might be explained by the potential belief by health care providers that the consent form for treatment signed by patients upon admittance serves as informed consent when faced with a procedure or medication, but that is not the case. Informed consent is a discussion between the health care provider and the patient prior to the treatment or procedure taking place.
If a doula or nurse were planning to leave their profession in the next three years, they were more likely to report observing disrespectful care. It has been long documented that people who support birthing people can experience secondary trauma after witnessing disrespectful care, especially if they feel powerless to intervene. Living the on-call life, and all the stress that comes with that, along with a deep respect for client-centered, respectful care of birthing people can create conflict when observing treatment that is considered disrespectful and demeaning.
One-third of all respondents reported observing verbal abuse in the form of threats to the baby’s life. Doulas were significantly more likely than nurses to report this behavior occurring occasionally or often. Since both doulas and nurses reported witnessing this threat, researchers assumed that respondents in both roles were able to distinguish between a truly emergent situation where concerns about fetal status are valid compared with when the threat is empty (the researches referred to this as the “dead baby card”) and used as a coercive mechanism to obtain compliance. This assumption seems to be validated by the fact that two-thirds of respondents report occasionally or often witnessing failures to obtain informed consent.
While there were few doulas and nurses of color in the study, they had significantly greater odds of reporting that they occasionally or often observed racially degrading remarks. The effects of formal education suggest that more education may increase awareness of racial/ethnic biases in maternity care.
Professionals who had given birth themselves reported witnessing threats, sexist remarks, and violations of informed consent more often than professionals who had not given birth. Possibly, a previous personal birth experience may result in a greater sensitivity to disrespectful behaviors. Does this make the doula or nurse more empathetic?
Doulas, simply by the definition of the doula role, have extremely limited options to bring about changing disrespectful behavior by a health care provider. Additionally, while the doula may feel the behavior is disrespectful, the perception of the client may be different. Nurses, as hospital employees, may have more influence in being change agents in the labor and delivery unit. The study did not examine the perception of the client or patient.
Doulas may also observe the nurse providing disrespectful care, especially for their clients of color who often receive different treatment based on their race or ethnicity. This is very hard to witness and observe for a doula. Doulas may have a hard time separating the doctor or midwife’s behavior from the L&D nurse’s care. This was not examined in this study.
For any doula who is working in a labor & delivery room, there may be times where they feel that the care being provided to their client is disrespectful, rude, threatening or worse. At times, the client’s perception may be similar, and sometimes not. Previous experiences, both personal and professional, by the doula along with other factors can influence these perceptions. Observing disrespectful behavior seems to contribute to a reduced desire to continue to work as a doula. The work doulas do is often described as “soul work” and the emotional impact is considerable, along with all the other stresses, including low pay, on-call lifestyles and finding a work-life balance that a doula must handle.
This study takes a deep dive into capturing the perceptions of doulas and L&D nurses witnessing disrespectful care by health care providers during labors and births. Many factors influence this perception. How do you feel about the care you witness being provided to your clients? Have your perceptions changed? What are you influenced by? How do you handle the emotional toll of observing this behavior? Let’s have a respectful conversation around this topic. Please remember to respect client confidentiality at all times.



Oh my goodness! I could not have read this at a better time! I am in weekly counseling for PTSD, severe depression, and severe anxiety! I have just in the last three month decided I need to sue the hospital where I worked as a Labor and Delivery nurse! I worked there in L&D for twelve years and would have worked there my whole career! I was intimidated to quit by a click of nurses that included my supervisor and two other nurses! I witnessed what I felt was a cover up of a babies death! There was a law suit but I do not know the out come! I do know those same two nurses were not reprimanded, as far as I have knowledge of! They were all still there when I transferred to another department a year or so later! When the baby death occurred the Labor and Deliver unit was divided! The click felt one way, and I believe most of the other nurses felt that the death could have been avoided! We had closed session meetings! We were instructed by the Mediators that there would not be retaliation for our opinion or what we said or felt! I for one was very angry and emotional about the babies death and the way these two nurses had treat the mother, the delivery, and the ultimate death of the baby! I had experienced the death of my own newborn years earlier! She was born April 1st 1996 and died April 30th 1996! During the time my baby girl was alive and in the NICU at PSL in Denver and then transferred to OB at our local hospital, I observed the care I and my baby received! Witnessing this care had caused me to become a L& D nurse! I wanted to be there when mothers and their families went through traumatic times like death or extremely unstable babies! I became a L& D nurse in 2000 and worked there full time until 2012 when I was intimidated by this same supervisor into stepping down from my position! I changed departments! I have experienced ( what I now understand to be) PTSD, severe depression and severe anxiety! I had to take a leave of absence from my position as Oncology RN Navigator in April of 2016! I had worked in the position from 2012 to 2016! Again HR was intimidating in their treatment of me! I left the hospital I had worked at for sixteen years due to these symptoms! I have tried to return to work as an RN several times in different jobs, only to have to step down due to these symptoms! I truly appreciate this artical! The artical helps me to realize I am not the only victim of this sad situation! Thank you for the opportunity to share my story as it has been very therapeutic!
I can’t even imagine! My heart goes out to you.
This topic is very hard. I experienced some of these in my own deliveries, and in those I assist as a doula. What is the proper thing for us to do in these situations?