By Sharon Muza, BS, CD(DONA), BDT(DONA), LCCE, FACCE, CLE
The American College of Obstetricians and Gynecologists (ACOG) released an updated committee opinion last month titled Optimizing Postpartum Care. This opinion was endorsed and supported by fellow maternal-infant health organizations that include the Academy of Breastfeeding Medicine, the American College of Nurse-Midwives, the National Association of Nurse Practitioners in Women’s Health, the Society for Academic Specialists in General Obstetrics and Gynecology, and the Society for Maternal–Fetal Medicine.
Before this new committee opinion had been released, current recommendations and community standards for postpartum medical visits for a birthing person under the care of an obstetrician were one visit at approximately six weeks post-birth. Birth and especially postpartum doulas working with families in the fragile days and weeks after birth have long recognized the need for quality support and care from a unified team of people, including family, doulas, friends, and health care providers. So much could and does happen in those first six weeks that lay the groundwork for future emotional and physical situations and challenges.
This newest statement acknowledges these challenges and the importance of ongoing support in this fragile time. The statement includes the following:
- To optimize the health of women and infants, postpartum care should become an ongoing process, rather than a single encounter, with services and support tailored to each woman’s individual needs.
- Anticipatory guidance should begin during pregnancy with development of a postpartum care plan that addresses the transition to parenthood and well-woman care.
- Prenatal discussions should include the woman’s reproductive life plans, including desire for and timing of any future pregnancies. A woman’s future pregnancy intentions provide a context for shared decision-making regarding contraceptive options.
- All women should ideally have contact with a maternal care provider within the first 3 weeks postpartum. This initial assessment should be followed up with ongoing care as needed, concluding with a comprehensive postpartum visit no later than 12 weeks after birth.
- The timing of the comprehensive postpartum visit should be individualized and woman-centered.
- The comprehensive postpartum visit should include a full assessment of physical, social, and psychological well-being.
- Women with pregnancies complicated by preterm birth, gestational diabetes, or hypertensive disorders of pregnancy should be counseled that these disorders are associated with a higher lifetime risk of maternal cardiometabolic disease.
- Women with chronic medical conditions, such as hypertensive disorders, obesity, diabetes, thyroid disorders, renal disease, mood disorders, and substance use disorders, should be counseled regarding the importance of timely follow-up with their obstetrician–gynecologists or primary care providers for ongoing coordination of care.
- For a woman who has experienced a miscarriage, stillbirth, or neonatal death, it is essential to ensure follow-up with an obstetrician–gynecologist or other obstetric care provider.
- Optimizing care and support for postpartum families will require policy changes. Changes in the scope of postpartum care should be facilitated by reimbursement policies that support postpartum care as an ongoing process, rather than an isolated visit.
There is a lot to like in these recommendations. For many people, the time period in the immediate days and first weeks after giving birth can be dangerous and often life-threatening. This is especially true for people of color. Sixty-one percent of deaths related to childbirth occur in the postpartum period and most of those occur in the first 42 days after birth (MacDorman, Declercq, Cabral, & Morton, 2016). Currently, 41 percent of postpartum people do not attend any postpartum visit. For families of color, this number is even higher.
Discussion prenatally about planning for the postpartum period is critical so that expectant parents can prepare and have in place the support they will need after childbirth. These new recommendations support those prenatal discussions and ask that they occur at several points during prenatal care. (SM note: how that is possible with the limited amount of time designated for a typical prenatal visit is unclear to me.) 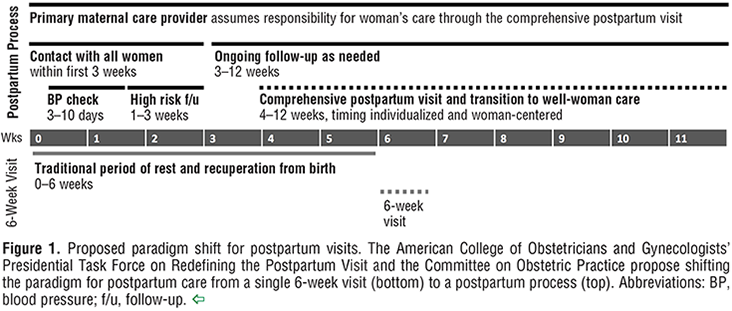
ACOG recognizes that emotional and physical complications are more likely to arise and remain when adequate support is not available postpartum. The Committee Opinion also identifies some of the barriers that currently exists for families who are not receiving appropriate postpartum care, including a quick return to work, lack of clarity on when and how to contact a provider for postpartum complications and even a lack of education provided before hospital discharge about circumstances that may arise that require contact with their provider.
One thing that is completely missing in this revised statement on Optimum Postpartum Care is the role of the postpartum doula. This trained professional can make an incredible difference in the lives of a new family, helping them to navigate the early days and weeks with confidence and unbiased support. ACOG needs to recognize that a postpartum doula can help ease the transition, encourage families to seek medical care when situations arise and be a valuable source of community resources of all sorts that families can access.
In the last two major committee opinions on birth, Safe Prevention of the Primary Cesarean and the newer Approaches to Limit Intervention during Labor and Birth, ACOG has recommended the presence of birth doulas as a method to improve maternal-infant health. This is to be applauded. Birth doulas are being recognized for their contributions to birth outcomes. The time has come for the same recognition to be made about postpartum doulas. This new committee opinion was the perfect document to include this statement, but unfortunately, the opportunity was missed. Postpartum doulas play a critical role in supporting families during the transition to parenthood.
ACOG designates who the players are on the “Postpartum Care Team” but postpartum doulas are nowhere to be found.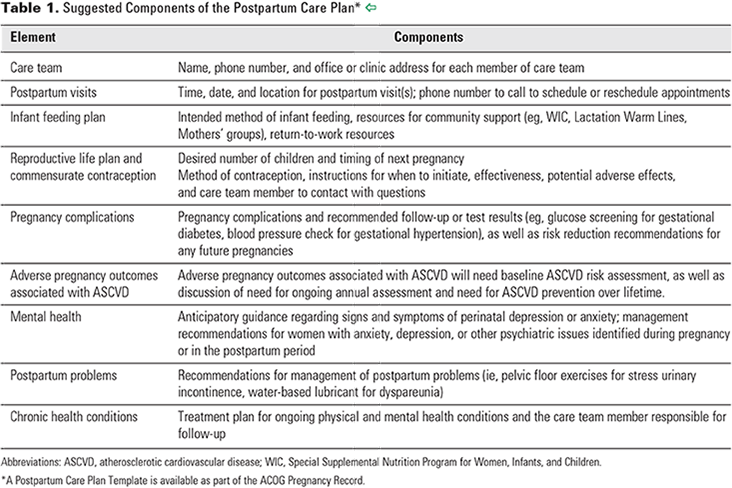
The time is now to recognize the valuable role that postpartum doulas have in the childbearing year. DONA continues to train and certify qualified individuals to serve in this role, providing valuable and necessary skills applicable to all families. Postpartum doulas deserve a place at the table and to be recognized for their valuable contributions to families after the birth of a baby.
References
Approaches to limit intervention during labor and birth. Committee Opinion No. 687. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;129:e20–8.
MacDorman, M. F., Declercq, E., Cabral, H., & Morton, C. (2016). Recent Increases in the US Maternal Mortality Rate: Disentangling Trends From Measurement Issues. Obstetrics and gynecology, 128(3), 447-455.
Optimizing postpartum care. ACOG Committee Opinion No. 736. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;131:e140–50.
Safe prevention of the primary cesarean delivery. Obstetric Care Consensus No. 1. American College of Obstetricians and Gynecologists.


As an Advanced Postpartum Doula and Postpartum Doula Trainer, I couldn’t have said it better myself; “The time has come for the same recognition to be made about postpartum doulas.” It’s disappointing to not yet receive backing from organizations such as ACOG, but I am so proud and grateful that DONA International advocates for and educates the public about the importance of our work! With our continued efforts, we will someday achieve the mission of providing a (postpartum) doula for every person who wants one.
I second Krista’s sentiments as well! Thank you DONA. The time has come for all of us DONA trained/certified PPDoulas to have our efforts validated by ACOG and many others.
Doulas, even trained doulas, are not medical professionals. There is no reason to expect ACOG to include them.
Anyone can call themselves a doula. Although DONA is a respected training organization, not all doulas are trained through them. Many patients call their labor support person a doula to get her in the room.
If they include birth doulas in their recommendations they can do the same for postpartum doulas now as well. Both are non medical professionals.