The contributions of doulas and the value of the support we provide has been recognized in 2014 in a joint statement by the American College of Obstetricians and Gynecologists (ACOG) and Society for Maternal-Fetal Medicine, and this year by the California Maternal Quality Care Coalition. Their focus is on the role doulas play during labor and birth. The benefits of postpartum doula support have not been as well noted. For example, a recent Committee Opinion by ACOG on Optimizing Postpartum Care leaves doulas out completely.
The Opinion states:
In the weeks after birth, a woman must adapt to multiple physical, social, and psychological changes. She must recover from childbirth, adjust to changing hormones, and learn to feed and care for her newborn (1). In addition to being a time of joy and excitement, this “fourth trimester” can present considerable challenges for women, including lack of sleep, fatigue, pain, breastfeeding difficulties, stress, depression, lack of sexual desire, and urinary incontinence (2–4).
— Committee Opinion: Optimizing Postpartum Care, ACOG
She needs a doula! Of course, a postpartum doula would not provide guidance, diagnosis or treatment for medical conditions such as incontinence or depression, but she can provide information to help the mother know if her symptoms warrant follow-up with a care provider and offer resources. A doula can have a tremendous impact on the other areas outlined by ACOG above, and leaving this role out of the care team seems like a significant disservice to families.
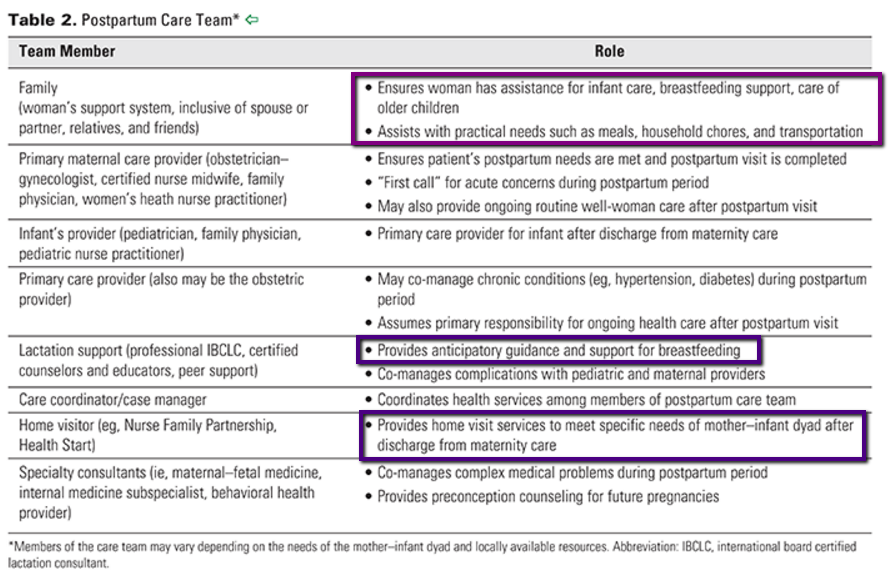
Let’s look at the care team as outlined by ACOG and the role of each member (boxes added):
The postpartum care plan outlined in the Committee Opinion relies heavily on family and friends to provide critical support for breastfeeding, meals, sleep, household responsibilities and care for older children. Because few people in America live near extended family and may move several times in their adult lives, it seems impractical to rely solely on family and friends for postpartum support, particularly over an extended period of time. ACOG appears to also assume that family and friends are both knowledgeable and supportive of breastfeeding, which may not be the case.
Lactation counselors and breastfeeding peer support are included in ACOG’s overview of the postpartum support team, which is an important step in normalizing breastfeeding and ensuring families are encouraged to seek support when questions or challenges arise. Doulas who are also certified lactation counselors may be in a better position to educate care providers and their community about postpartum doulas given the inclusion of certified lactation support providers in this Opinion. ACOG previously issued a statement strongly encouraging care providers to play a more active role to support breastfeeding, both in their care practices and in policymaking. It stands to reason that emphasis on the support doulas provide for breastfeeding would be well received by care providers.
Home visitors are also included in the care team as outlined by ACOG, highlighting the importance of having support come to the family and see them in their own environment. This may be the least recognized value of postpartum doulas. While doulas, of course, do not provide the services a home visiting nurse or social worker would to address medical or other challenges, the hands-on support, continuity of care, and training a postpartum doula brings into the home is extremely valuable to the new family.
To be fair, the Committee Opinion on Optimizing Postpartum Care, like nearly all publications from ACOG, focuses heavily on medical care, and doulas do not provide medical care of any kind. Yet this Opinion also covers areas that absolutely fall under the scope of support provided by professionally trained and certified doulas. The exclusion of professional doulas from the postpartum care team seems like a significant oversight given the role and impact of doula support in the fourth trimester.
ACOG is clear that care providers must use their own discretion to determine the course of action for each individual patient, and so their Committee Opinions and Practice Updates are not “rules” by any means. Yet the organization is a powerful voice in the maternity care field, and their guidelines can sometimes drive policy decisions at care practice offices and hospitals. Their acknowledgement of doulas – both birth and postpartum – as members of a family’s professional care team would go a long way to support care provider acceptance and understanding of our role as well as greater utilization of doulas by families.
For more on the types of documents they release and the speed at which changes tend to be adopted by care providers, check out our article on Understanding ACOG Updates.
— Adrianne Gordon, MBA, CD(DONA)



I think finding medical evidence for postpartum doula care is difficult to find, and that is ACOG and SMFM’s staple for creating opinions. Most of the evidence for PP support comes from studies that include several elements of PP support – case managers, nurses. LC’s, and doulas. Doulas who work for community based programs often have multiple responsibilities: lactation counselors, educators, drivers, at minimum. Long standing programs have perinatal community health workers (PCHW) offer doula services, which enables them to offer better wages and expanded services to clients. In other words, the postpartum care models where there is research either do not separate out postpartum doula services from other services offered to clients, or do not use doulas to fulfill the functions of postpartum support. We do have good qualitative evidence that postpartum doula support enhances the mother’s experience and adds to good breastfeeding outcomes, but no quantitative or statistical evidence that shows the impact. No one has ever done a matched pair study or randomized trial comparing people who had PP doula support with those who did not.
I also noticed that every position on the list besides family was either licensed or had layers of entrenched oversight (case manager, home visitor). Postpartum doulas are paraprofessionals who would work with any of these other roles, and do so mostly as independent contractors. I wonder if they decided not to mention independent paraprofessionals because there is no consumer protection, licensing, or any control over the health care messages that might be given to a vulnerable family.