It’s no secret that the health of women after they give birth in the United States is declining rather than improving. Both rates of death (mortality) and complications (morbidity) are on the rise. In a 2015 Bulletin, the World Health Organization stated the situation clearly:
Between 1990 and 2013, the maternal mortality ratio for the USA more than doubled from an estimated 12 to 28 maternal deaths per 100,000 births (1), and the country has now a higher ratio than those reported for most high-income countries and the Islamic Republic of Iran, Libya and Turkey.(2) About half of all maternal deaths in the USA are preventable.(2)
Each year an estimated 1,200 (1) women in the USA suffer complications during pregnancy or childbirth that prove fatal and 60,000 (3) suffer complications that are near-fatal – even though costs of maternity care in the USA in 2012 exceeded 60 billion United States dollars.(4)
— Maternal Mortality and Morbidity in the United States of America, Bulletin of the World Health Organization
The trend for increased deaths and complications from birth, coupled with the high cost of health care, were a driving factor in the creation of the Congressional Maternity Care Caucus DONA International participated in late last year. Since 2012, the American Congress of Obstetricians and Gynecologists (ACOG) and the Centers for Disease Control (CDC) have come together for an annual joint meeting on maternal mortality and morbidity to share updated research and resources.
Rising Complications & Measurement Challenges
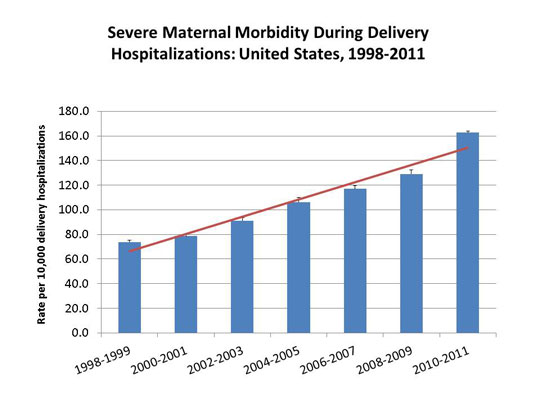
Late last year, ACOG and the Society for Maternal-Fetal Medicine (SMFM) issued their fourth joint statement in the Obstetric Care Consensus Series, entitled Severe Maternal Morbidity: Screening and Review. They focused on severe maternal morbidity saying, ”….severe maternal morbidity can be thought of as unintended outcomes of the process of labor and delivery that result in significant short-term or long-term consequences to a woman’s health.”
Source: CDC.gov
One of the challenges in evaluating the overall trend for worsening outcomes for women is that there is no set definition of the term ‘severe maternal morbidity’. Without agreed upon parameters on what constitutes an outcome with “significant” health impacts, care providers and hospitals nationally aren’t on the same page about what should be reviewed or measured. ACOG and SMFM say that setting a definition is beyond the scope of their current statement but that it may be the basis of future work for the two organization that guide a majority of maternal care providers. ACOG and SMFM highlight the importance of reviewing maternal morbidity patient cases in their joint statement saying, “The purpose of identifying and evaluating these cases is to facilitate opportunities for improvement in care.”
Increasing Death Rates & More Measurement Challenges
Maternal death is defined as death of a pregnant woman or one who has given birth with 43 days, according to the World Health Organization. In 2003 the standard U. S. death certificate was amended to add questions to better measure maternal death including expanding the timeframe by giving coroners the option to indicate if the woman had been pregnant within the last year. States adopted the practice somewhat sporadically if at all. As a result, the U.S. has not published an official maternal mortality rate since 2007. Recent news headlines about rising mortality rates have come as a result of research published in ACOG’s journal Obstetrics & Gynecology in September 2016 evaluating the available data. The authors concluded:
The estimated maternal mortality rate (per 100,000 live births) for 48 states and Washington D.C. (excluding California and Texas, analyzed separately) increased by 26.6%, from 18.8 in 2000 to 23.8 in 2014. California showed a declining trend, while Texas had a sudden increase in 2011–2012. Analysis of the measurement change suggests that U.S. rates in the early 2000s were higher than previously reported.
— Recent Increases in the U.S. Maternal Mortality Rate: Disentangling Trends From Measurement Issues. Obstetrics & Gynecology
Additional research is needed to evaluate the data from the state of Texas further. The article notes that several women’s health clinics closed there, but that the increase was was more likely to results in other factors including possibly change to how maternal deaths were reported. The authors noted that increases of this magnitude seem unlikely without significant external factors such as war or natural disaster.
California is a bright spot in the results with the efforts, tools, and evaluation of cases lead by the California Maternal Quality Care Collaborative highlighted as supporting this large state’s increases safety for birthing women.
Resources to Learn More
Measurement challenges aside, the declining trend in outcomes for women after they give birth is very real. We expect much more research and statements from the maternal health field on both mortality and morbidity in the future. If you’d like to learn more about outcomes after birth or find out who is working to address these challenges, these resources are available. If you know of others, let us know and we’ll update this list.
Science & Sensibility – Our friends over at Lamaze International have been digging deep into this topic including a five part article series entitled “Maternal Morbidity and Mortality in the United States: Where do we go from here?”
Alliance for Innovation on Maternal Health – a program of the Council on Patient Safety in Women’s Healthcare has created patient safety tools and bundles in addition to quality improvement competitions. This program was previously called the National Partnership for Maternal Safety.
California Maternal Quality Care Collaborative – a non-profit focused on morbidity, mortality and racial disparities in maternity care. CMQCC’s work is credited with helping improve maternal health outcomes in California. The collaborative has expanded and now provides resources like toolkits and data center for maternity care providers nationally.
2016 ACOG-CDC Annual Maternal Mortality and Severe Maternal Morbidity Meeting – These meetings are open to the public and the agenda and select presentations are available online.
CDC Severe Maternal Morbidity in the United States – The CDC’s official page on this topic provides their definition as well as trend data and additional references.
MacDorman, Marian F. PhD; Declercq, Eugene PhD; Cabral, Howard PhD; Morton, Christine PhD. Recent Increases in the U.S. Maternal Mortality Rate: Disentangling Trends From Measurement Issues. Obstetrics & Gynecology, August 2016 DOI: 10.1097/AOG.0000000000001556
D’Alton et al. National Partnership for Maternal Safety. Obstetrics & Gynecology, May 2014 DOI: 10.1097/AOG.0000000000000219



I fear the rising death rate is due to the following situations: women who can afford the services of births with private OBGyns, nurses, midwives, and doulas now birth in clinics or at home; whereas women of lower socioeconomic status go to hospital and are served with less attention. Further, a good number of these women are of darker skin tones; the lesser care given darker women and clients/patients with any need for hospitalization has been studied and recorded many times. The resulting outcome is that good health care is only afforded by the white upper middle and upper class citizens. Population-wise there are fewer. The percentage of the underserved is alarmingly high, in a country where health is not viewed as a national goal which the government must undertake!