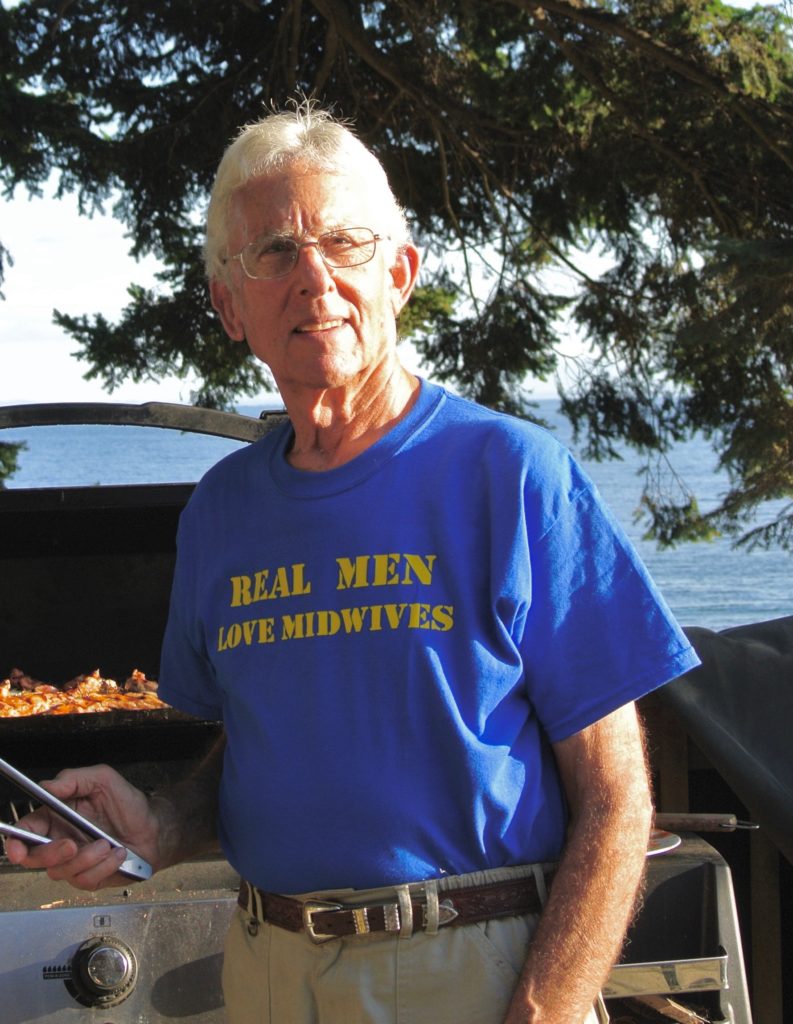
By Michael Klein, MD
Dr. Marshall Klaus passed away on August 15, 2017, at the age of 90. Dr. Klaus was one of DONA International’s founders and a leader in maternal-infant bonding. We have covered Dr. Klaus’ death previously on the blog. This past weekend, there was a memorial for Dr. Klaus in his hometown of Palo Alto, and many leaders of maternal-infant health traveled there to honor Dr. Klaus and his contributions to childbearing families. Dr. Michael Klein- Family Physician, Pediatrician, Neonatologist and Maternity Care Researcher was one who made the trip, and he has generously shared his tribute with all of us here at DONA International. Every time I read more about Dr. Klaus, I am sorry that I did not have a chance to know him and work with him. He was simply amazing! – Sharon Muza, Blog Manager, DONA Doula Chronicles.
Marshall Klaus was a key mentor in my life, known for his work on maternal-newborn bonding, and one of the founders of the doula movement. At the celebration of his life in Palo Alto, California on Nov 4, 2017, many tributes were offered. I spoke of him in the following way:
I met Marshall for the first time as a medical student at Stanford in 1965. I had just returned from a one and half year leave of absence from the medical school, having worked in a pediatric hospital in Addis Ababa Ethiopia, where I had been given more responsibility than was usual for a student. Now back at Stanford, they were using me as a resident.
One night on duty, alone in the small neonatal ICU run by Philip Sunshine, I became increasingly concerned about the well-being of a 1500 gram premature infant in respiratory distress. His condition was deteriorating. It was becoming more and more difficult for me to maintain the infant’s oxygen level. I had reached the limit of what the respirator and my knowledge could do. Knowing that I needed help, I looked on the list of covering attending physicians. The day’s attending physician was Marshall Klaus. I had never heard of Dr. Klaus, who had come to Stanford while I was in Ethiopia. At about 3 am, I called Dr. Klaus. He shambled in. Marshall always shambled, in part because of his residual weakness dating from polio acquired by caring for children in a polio epidemic. I speculate now that Marshall’s empathy for mothers, babies and many others may be as a result of his experience of disability. He would be shocked to hear me describe him as disabled. He never acknowledged his limitation. He just pushed through it.
At any rate, Marshall listened respectfully to my concerns. He examined the preemie and studied the blood gas results. Expecting some help, I was stunned to have him say: “What do you think this baby is thinking?” I don’t remember exactly what I said but I might have been a bit rude.
Marshall then said: “How do you think this baby’s mother felt when she had to go home and leave her baby behind?” I am sure that my response was less than positive. But I do remember vividly what he next said: “Sadly, this baby is going to die and there is nothing further that we can do for him. Let’s think about what we can learn about him to help his unfortunate mother.”
Wrong time for me to hear this. I could not relate to Dr. Klaus. I was still in cure mode, likely based on my age and the Ethiopian experience. Dr. Klaus was looking at the big picture. Developmentally I was not on the same page as Dr. Klaus, but it was not too many years later that I was consulting him regularly and had come to deeply appreciate his great contributions to the field of maternal-newborn well-being.
That night, I didn’t know that he was deeply involved with Dr. John Kennell in early attachment research and about to publish one of the first studies on maternal-infant bonding. At that time, he was germinating the work that was to lead to a seminal article in Pediatrics in 1970 called: “Neonatal separation: the maternal side of interactional deprivation.”
Marshall’s genius was to reinvent himself on a regular basis. He originally was a pediatrician and pediatric respirologist and newborn specialist. His early publications from the 60s were on the newborn lung and newborn respiratory problems—not a whiff of bonding.The discipline of neonatology has not even been formally invented as a subspecialty of pediatrics until 1975.
Believe it or not, in 1975, I was sitting beside him in Philadelphia, where we were both writing the first exam for the newly recognized sub-specialty of neonatal-perinatal medicine. I had been studying his book on newborn respiratory disease in preparation for the exam. The student and teacher were now colleagues.
By the 1980s, Marshall and John were writing and researching about what they called “a supportive companion.” In the 1990s they had published in JAMA an RCT of emotional support for what was later to be called a doula study.
Translating research into practice is something researchers yearn for. Marshall’s study of doulas led naturally to his work with Penny Simkin, Annie Kennedy, John Kennell and Phyllis Klaus to the formal creation of Doulas of North America (now called DONA International) and the doula movement–leading to monumental impact internationally.
Marshall’s impact came home to me in a strange and funny way in the late 1990s when Marshall, Sheila Kitzinger and I were invited to Mexico City by Mexican doulas who were trying to introduce doulas and other important changes to a military hospital, a hospital where the nursery was guarded by a soldier carrying a machine gun. We all gave talks earlier in the day, after which we were invited to meet with various staff members. Marshall and I were taken to the nursery where we saw more monitoring equipment than was present in most US hospitals. The mother labored on a fancy birthing bed in a huge elegant tiled room with lots of equipment.
But after the birth, the newborn was immediately transferred to be warehoused in a nursery. We were presented with the institutional problem of excess jaundice and infection rates. What did Marshall recommend? Without hesitation, Marshall opined to the hapless neonatologist in charge: “It’s easy, just have the mother labour in this large room and keep her baby with her ’til discharge, breastfeeding on demand. Don’t let others handle the baby. Your jaundice and infection will disappear.” The president of the hospital, who was a military general with lots of stars and gold braid, turned to the stunned neonatologist: “You have four months to get this done, or you will be looking for another job.” I am sure that Marshall and I would have loved to be a benevolent dictator. What changes we could make.
In the early 2000s, Marshall was writing about the range of interventions, many inappropriate for mother and newborn. He was particularly incensed by the over-use of epidurals.
One of his most beloved offerings, created with Phyllis Klaus, was the book Your Amazing Newborn, used by countless couples. Bonnie and I gave it as a present, as many others did, to our kids Seth and Naomi, when they were approaching their first births.
Throughout his life, I regularly consulted with Marshall. What studies to do? What measurements to use? Where to take a sabbatical? Or just hang out. I was a long way from the medical student who could not figure out what the hell he was talking about. I count Marshall as a key mentor who helped shape my own research–but more importantly, I count Marshall as a dear friend. His passing leaves a great gap that cannot be filled. He will live on in immediate skin-to-skin bonding, the disappearance of central-nurseries, replaced by universal-rooming-in and the ever-expanding role of the doula. Today, generations of mothers and fathers will experience a totally different connection with their newborns than those who gave birth in the 60s and 70s, and they won’t even know why. But we do.




He will be so missed. I am so grateful for his work and legacy on behalf of mothers and babies. Thank you, Dr. Klein for such excellent words. Thank you for sharing, Sharon.